Joint replacement surgery, whether for a knee, hip, or shoulder, is a huge milestone. For many in Ottawa, it signals the end of chronic, debilitating pain and the promise of restored mobility. You’ve successfully navigated the preoperative planning, the procedure itself, and the challenging early weeks of rehabilitation. You might feel like you’ve finally kicked osteoarthritis (OA) to the curb. However, it’s crucial to understand that surgery, while transformative, isn’t always the final destination in managing a chronic disease. In fact, comprehensive osteoarthritis care remains essential for a successful, long-lasting recovery and overall joint health.
This article will walk you through why a proactive, long-term approach to managing OA symptoms and supporting your musculoskeletal system is vital post-operation. We’ll explore the essential strategies, from advanced rehabilitation techniques to orthopedic supports, that can protect your new joint, manage residual or referred pain, and ensure you maintain the fantastic results you worked so hard to achieve. We know you want to get back to walking the paths along the Rideau Canal or enjoying the Gatineau Hills, and the right care plan will help you do just that.
Why Joint Surgery Isn’t the End of the Road for Chronic OA
Osteoarthritis is a chronic, progressive condition that affects not just the joint cartilage, but the entire joint structure, including bone, ligaments, and muscle. While a total joint replacement (arthroplasty) removes the damaged joint surfaces and eliminates the primary source of pain in that specific area, it doesn’t cure the underlying disease process.
Here are a few reasons why continued vigilance and specialized care are non-negotiable after your operation:
1. The Adjacent Joint Effect
The new joint is stable, but the surrounding joints, like the ankle and hip after a knee replacement, or the other knee, have been compensating for years due to your pre-operative pain and stiffness. That compensatory movement pattern often puts excessive stress on these adjacent areas. This phenomenon, known as the “adjacent segment disease“ or effect, can accelerate OA progression in other areas. Therefore, a key part of continued care is ensuring optimal alignment and biomechanics across your entire body to protect these vulnerable areas.
2. Muscle Atrophy and Strength Imbalances
Even with intensive physiotherapy, it takes months, and sometimes years, to fully restore the muscle strength and control surrounding the operative joint. The muscles were likely deconditioned and imbalanced long before the surgery. Regaining this deep stability and endurance is essential. Without robust muscle support, the strain transfers back to ligaments and the prosthetic components themselves, potentially impacting the implant’s longevity. Furthermore, strengthening your core and the stabilizing muscles around your spine is also integral for supporting the lower body joints.
3. Referred and Residual Pain Management
While the primary pain source is gone, many patients experience residual nerve or muscle pain, or pain referred from the lower back or adjacent joints. A long-term osteoarthritis care plan must incorporate advanced pain management techniques that move beyond early post-operative medications. These techniques include targeted dry needling, nerve gliding exercises, and non-pharmacological methods like heat, cold, and TENS (Transcutaneous Electrical Nerve Stimulation) units. This comprehensive approach is much more sustainable and effective for long-term comfort.

The Four Pillars of Long-Term Post-Op Osteoarthritis Care
A comprehensive, long-term care strategy is built upon four interconnected components that work synergistically to support your new joint and prevent secondary issues.
Pillar 1: Targeted Rehabilitation and Movement
This stage goes beyond the initial post-op physio. It’s about building durability. Your focus shifts from simply increasing the range of motion to achieving functional milestones like walking for longer distances, navigating stairs effortlessly, or returning to sports.
- Progressive Resistance: Gradually increasing resistance training to build muscle bulk and joint stability.
- Balance and Proprioception: Exercises that challenge your balance, which is often impaired after joint damage. Tai Chi and single-leg stands are excellent examples.
- Functional Training: Integrating movements that mimic real-life activities, such as squatting to pick up an object or stepping sideways.
Pillar 2: Weight Management and Nutrition
This is perhaps the simplest yet most challenging component. Every pound of body weight places four to six pounds of pressure on your knees and hips while walking. Losing even a small percentage of body weight can dramatically reduce stress on your prosthetic joint and your remaining joints.
- Anti-Inflammatory Diet: Focusing on foods rich in Omega-3 fatty acids, antioxidants, and fibre can help manage the systemic inflammation associated with OA.
- Supplementation: Consulting with a healthcare professional about supplements like Vitamin D and Calcium is essential for bone health, which supports the integration of the prosthetic.
Pillar 3: Orthopedic Supports and Biomechanical Aids
For many patients, especially those with multi-joint involvement, orthopedic supports, from off-the-shelf braces to specialized custom devices, are a foundational component of ongoing osteoarthritis care. Off-the-shelf options are often the best starting point for immediate support and relief.
- Off-the-Shelf Braces: These provide immediate stability and pain relief for minor to moderate symptoms in the adjacent joints, offering an affordable and accessible solution.
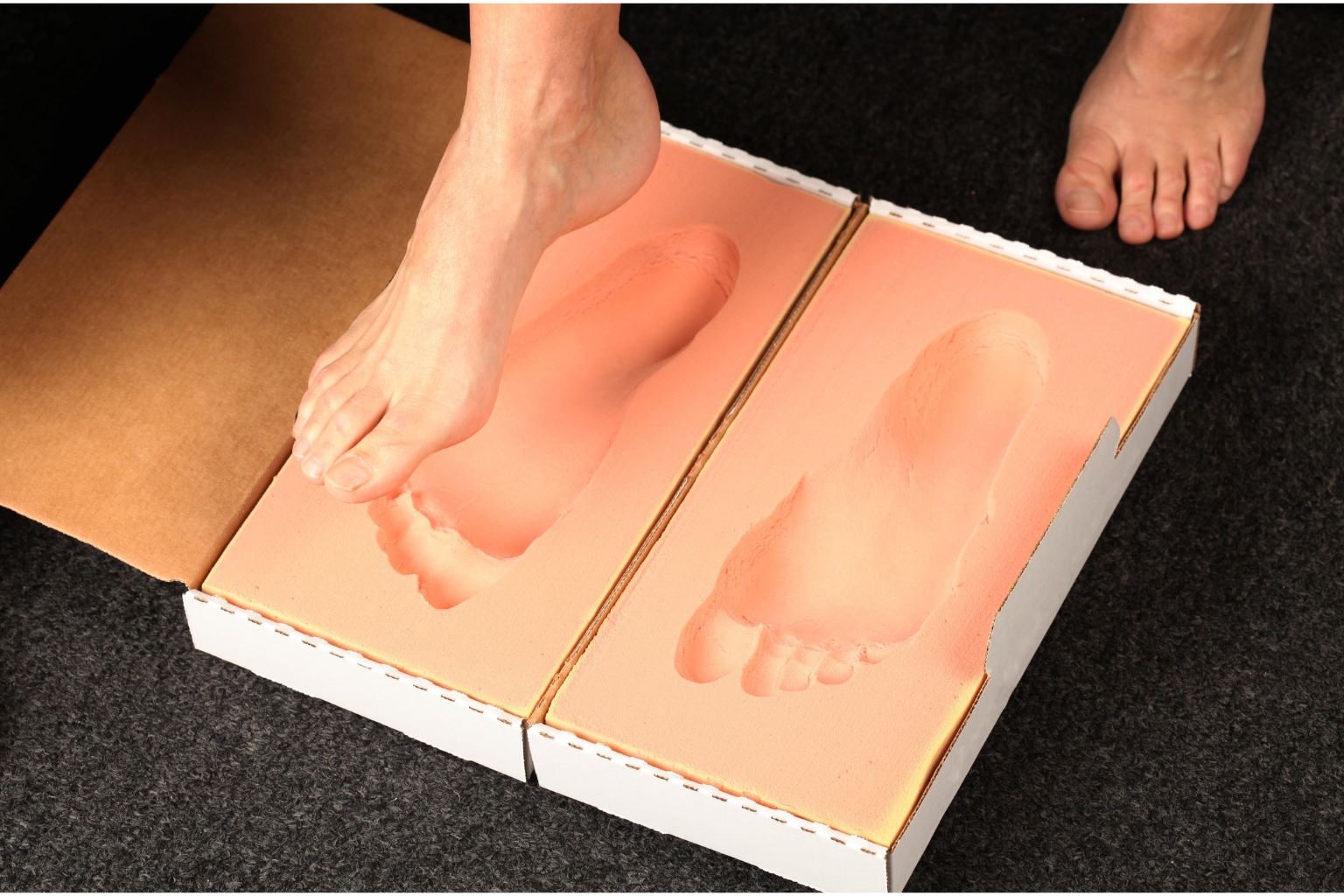
- Foot Orthotics: These adjust alignment at the ground level, which can significantly reduce rotational strain on the knees and hips.
- Specialized Supports: This includes custom unloader braces for severe adjacent joint OA or highly specialized supports for activity-specific protection.
Pillar 4: Regular Monitoring and Imaging
You shouldn’t wait for pain to return before seeing your orthopedic surgeon or physiotherapist. Regular check-ups are vital for monitoring the prosthetic and the surrounding soft tissues. Catching issues like component wear, subtle loosening, or early signs of OA in an adjacent joint can be addressed quickly, preventing major complications down the line.
Orthopedic Supports: Off-the-Shelf Solutions and KineMedics’ Expertise
If you’re in the Ottawa area, the need for personalized osteoarthritis care often leads to exploring orthopedic supports. KineMedics prioritizes finding the most effective solution for your needs, starting with highly effective, readily available off-the-shelf options.
Finding the Right Support Post-Surgery
- Precision and Alignment: Getting the right size ensures the support device correctly guides your joint alignment. This is critical for post-operative knees and hips, where even slight misalignment can create abnormal wear patterns on the implant.
- Protection of Compensating Joints: A professional assessment can determine the exact support needed. For instance, a high-quality knee sleeve might stabilize your gait enough to reduce stress on your hip, while a custom foot orthotic provides perfect ground-level stabilization.
- Enhanced Confidence and Mobility: Knowing you have a perfectly fitted, high-quality support can eliminate hesitation and fear of movement, allowing you to engage more fully in your rehabilitation and daily life. This boost in confidence directly translates into better functional outcomes.
The KineMedics team specializes in assessing your specific post-op biomechanics to determine the exact support necessary for your continued success. We consider your pre-existing conditions, your surgical history, and your lifestyle goals to recommend the most effective solution.
Your Ottawa, Ontario Recovery Journey: Entities and Resources
Focusing on your recovery right here in Eastern Ontario means understanding the resources available. When managing chronic conditions like OA, consistency and local accessibility matter greatly.
Key Entities in Your Recovery:
- Ottawa Physiotherapists: Provide specialized post-op protocols, progressive exercise guidance, and manual therapy to address muscle stiffness.
- Local Valley and Regional Hospitals (e.g., The Ottawa Hospital, Queensway Carleton, Montfort, Almonte General): Your surgical team provides crucial follow-up for the implant itself.
- KineMedics (Orthotic Specialists): Assessment and fitting of off-the-shelf and custom orthopaedic devices, ensuring ongoing biomechanical support.
By coordinating your care among these local professionals, you establish a strong safety net. Continuous, tailored osteoarthritis care is a partnership between you and your healthcare team, designed to maximize the lifespan of your replacement and keep you active for years to come. Remember, the goal isn’t just to recover; the goal is to thrive.

Frequently Asked Questions (FAQ) About Post-Op OA Management
We’ve found that patients transitioning from the intensive rehabilitation phase to long-term management often have similar questions. Here are concise answers to help guide your ongoing care:
Q: Can osteoarthritis still cause me pain after my joint replacement?
A: Yes, it can. While the pain from the severely damaged joint surface is gone, you may experience pain from surrounding tissues, referred pain from the spine, or from other joints that are now bearing a different load (like the non-operated knee or hip). This is why a targeted post-op pain management strategy is so important.
Q: How long does the “maintenance“ phase of physiotherapy last after surgery?
A: The formal, intensive physiotherapy phase usually lasts 3 to 6 months. However, the maintenance phase, where you continue prescribed exercises independently at home or in a gym, should ideally last for life. Think of your exercises not as therapy, but as non-negotiable joint protection. You should check in with a physiotherapist annually for tune-ups and progression of your exercise routine.
Q: Will my new joint last longer if I continue specialized care?
A: Clinical evidence strongly suggests that excellent post-operative care, particularly focusing on optimal muscle strength, body weight management, and alignment, contributes to the longevity of the prosthetic implant. Reducing impact forces and minimizing wear and tear on the polyethylene insert are direct benefits of comprehensive, ongoing osteoarthritis care.
Q: Is it safe to return to high-impact sports like running or skiing after a joint replacement?
A: Generally, high-impact activities are discouraged because they significantly increase the wear rate on the prosthetic components. However, this is highly individualized. It’s essential to discuss your specific goals with your orthopedic surgeon, physiotherapist, and bracing specialist. Low-impact activities like swimming, cycling, and walking are always recommended and strongly encouraged to maintain flexibility and strength.
I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.a
Take the Next Step in Your Long-Term Health
You’ve done the hard part, you’ve committed to surgery and started your rehabilitation. Now is the time to solidify those gains and invest in the future of your mobility. Long-term osteoarthritis care is the key to ensuring your joint replacement serves you well for decades to come.
If you’re ready to optimize your movement patterns, explore personalized bracing options for enhanced stability, or receive a thorough assessment of your post-operative biomechanics, the KineMedics team is here for you. We’ll help you develop a personalized plan that supports your new joint and protects the rest of your body, ensuring you maintain the active Ottawa lifestyle you deserve.